What does blood in stool look like? Noticing blood in your stool can be alarming, but it’s important to remember that it is a symptom, not a disease.
The color and appearance of stool blood can provide important clues about the cause. It may appear as bright red streaks, dark maroon, or black and tarry, each pointing to different areas of the gastrointestinal (GI) tract.
While minor issues like hemorrhoids or anal fissures are common causes, serious conditions such as infections, inflammatory bowel disease (IBD), or colorectal cancer can also lead to blood in stool.
In this article, you will learn about the different colors of blood in stool, common signs and symptoms, underlying causes, risk factors, and when to seek medical help.
Understanding these details helps you act promptly and protect your digestive health.
Common Appearances of Blood in Stool
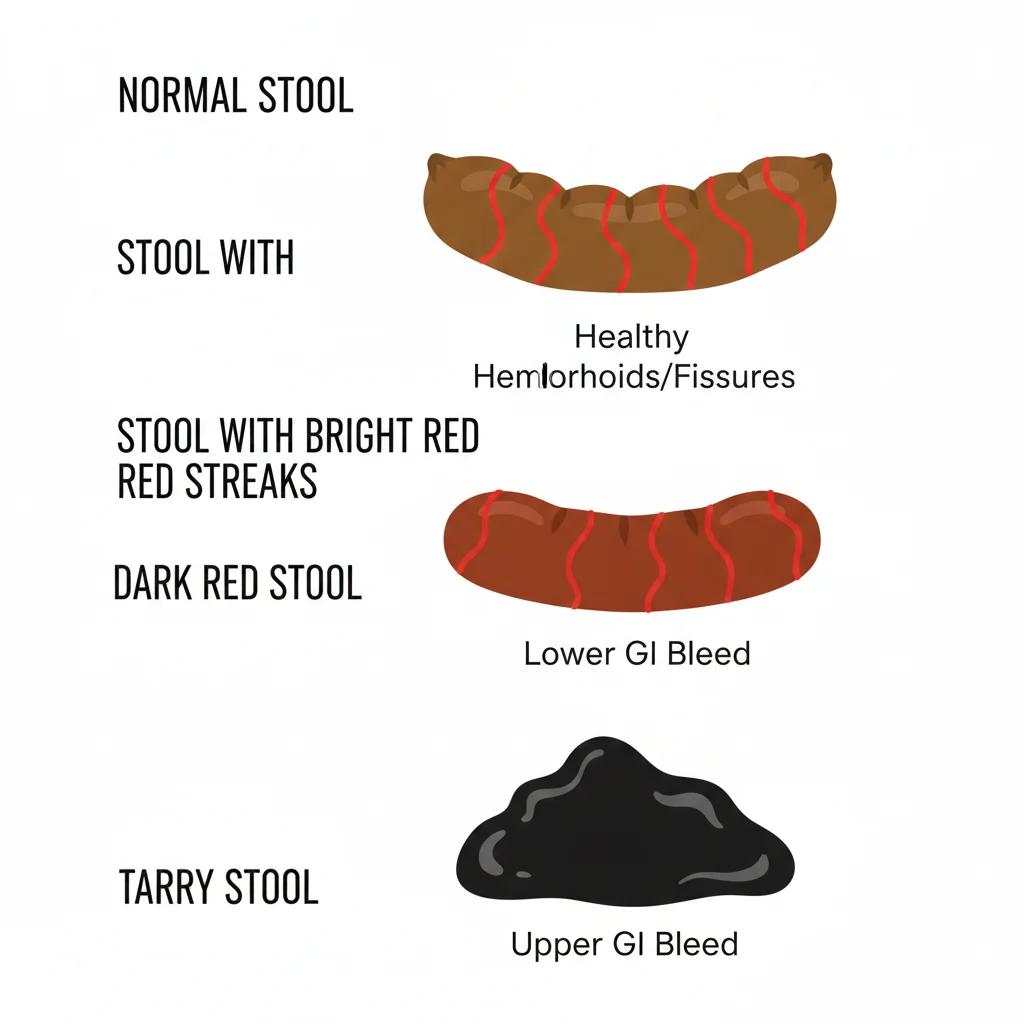
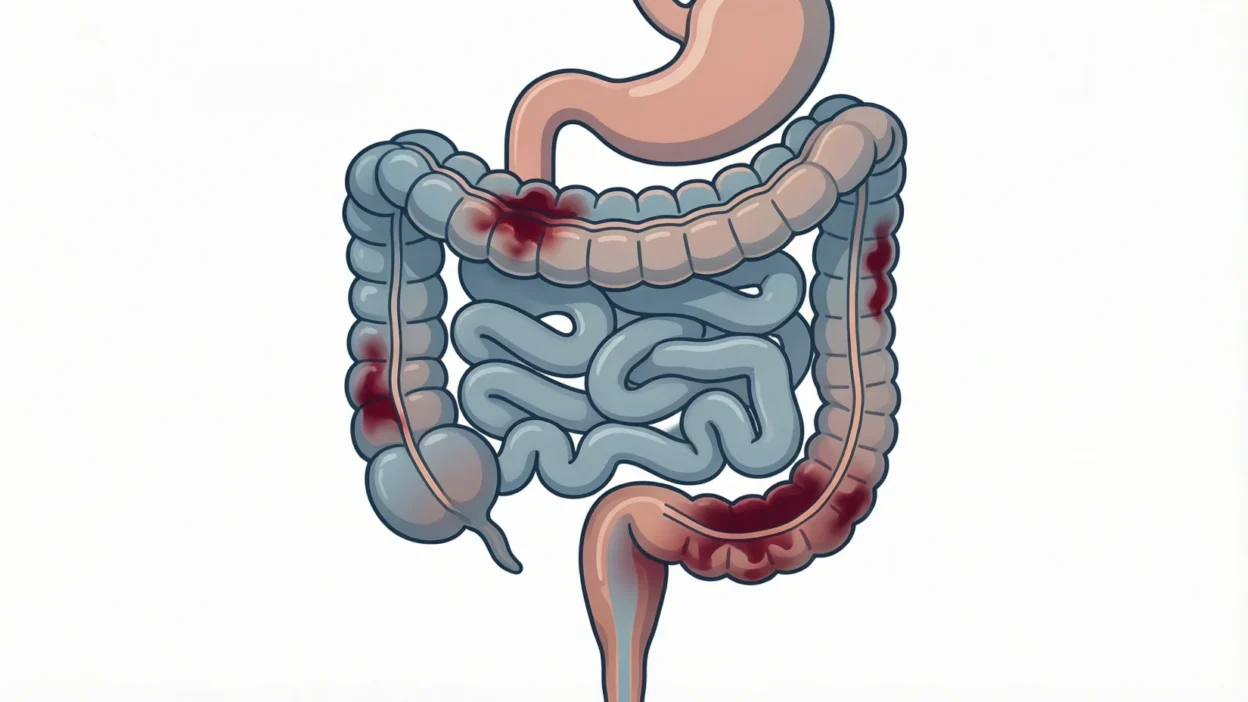
Blood in stool can vary significantly in color, texture, and amount, and these differences often indicate the location and cause of the bleeding. One of the most noticeable types is bright red blood, which usually comes from the lower gastrointestinal tract, such as the rectum or anus. This can appear as streaks on the stool, blood coating the stool, or blood on the toilet paper after wiping.
In contrast, dark red or maroon blood may come from the small intestine or upper colon, often indicating a slower bleeding source. Black or tarry stools, also known as melena, suggest that blood has been digested in the stomach or upper GI tract, and the stool may have a sticky texture with a strong odor. Sometimes, blood may appear as pink or lightly streaked, often a sign of minor bleeding such as from hemorrhoids or anal fissures.
Understanding these differences can help determine the urgency of medical evaluation and guide your next steps in care.
Causes of Blood in Stool
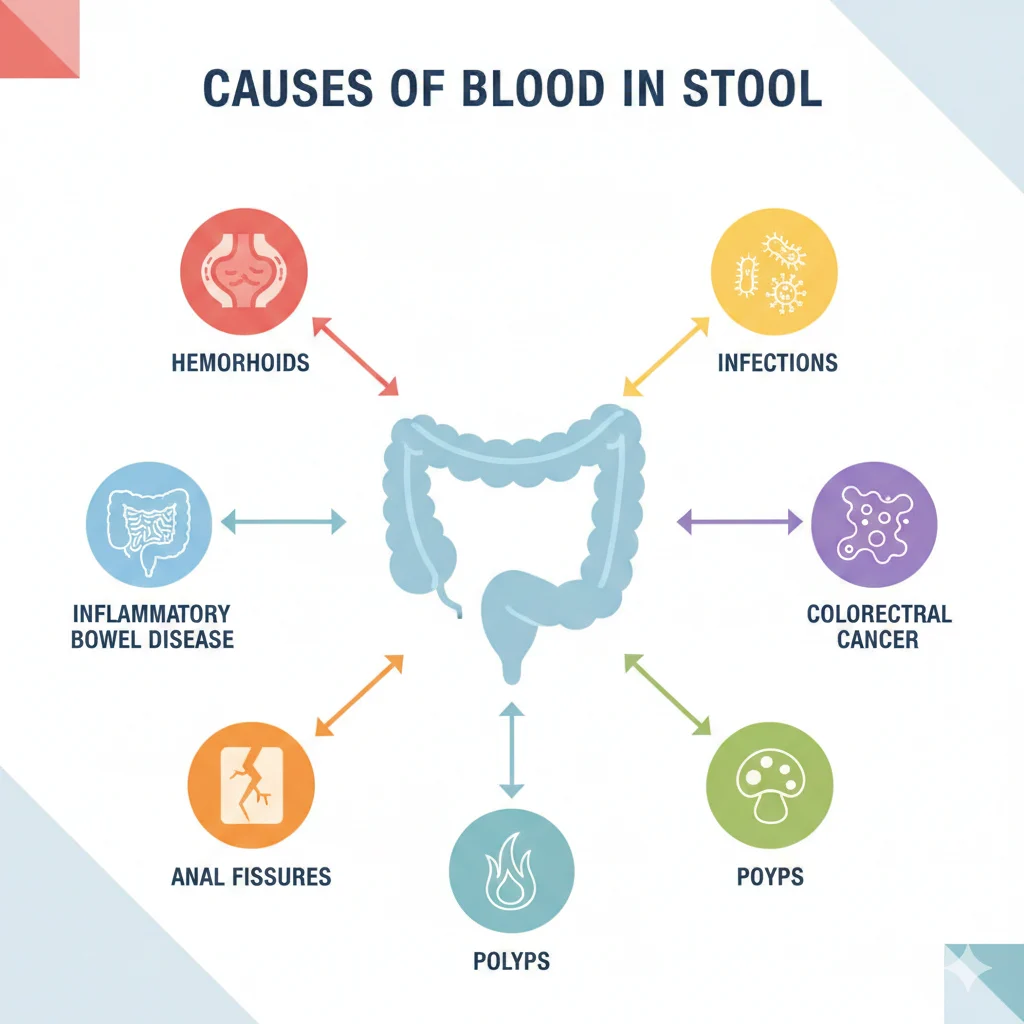
Blood in stool can be caused by a variety of conditions, ranging from minor issues to serious medical concerns. Understanding the possible causes can help identify the urgency and type of treatment needed.
Hemorrhoids and Anal Fissures
Hemorrhoids are swollen veins in the rectum or anus that can bleed during bowel movements, producing bright red blood on the stool or toilet paper. Anal fissures, small tears in the lining of the anus, can also cause similar bleeding, often accompanied by pain or a burning sensation during bowel movements.
Gastrointestinal Infections
Bacterial, viral, or parasitic infections can irritate the digestive tract, sometimes causing bloody diarrhea or mucus with blood. Common culprits include Salmonella, E. coli, and Shigella.
Diverticulosis and Polyps
Diverticulosis involves small pouches in the colon wall that may rupture, leading to sudden, painless bleeding. Colon polyps, abnormal growths, can also bleed slightly and may be precursors to colorectal cancer if left untreated.
Inflammatory Bowel Disease (IBD)
Conditions like Crohn’s disease and ulcerative colitis cause chronic inflammation in the GI tract. Blood in stool from IBD is often mixed with mucus, accompanied by cramps, diarrhea, and fatigue.
Cancer (Colorectal or Stomach)
Blood in stool can sometimes be a warning sign of colorectal or stomach cancer, especially if bleeding is persistent, dark, or accompanied by unexplained weight loss, fatigue, or changes in bowel habits.
Medications and Lifestyle Factors
Certain medications, like NSAIDs or blood thinners, can irritate the GI tract and cause bleeding. Lifestyle factors, including chronic constipation or straining, may also contribute to minor bleeding.
Color Variations and Their Meanings
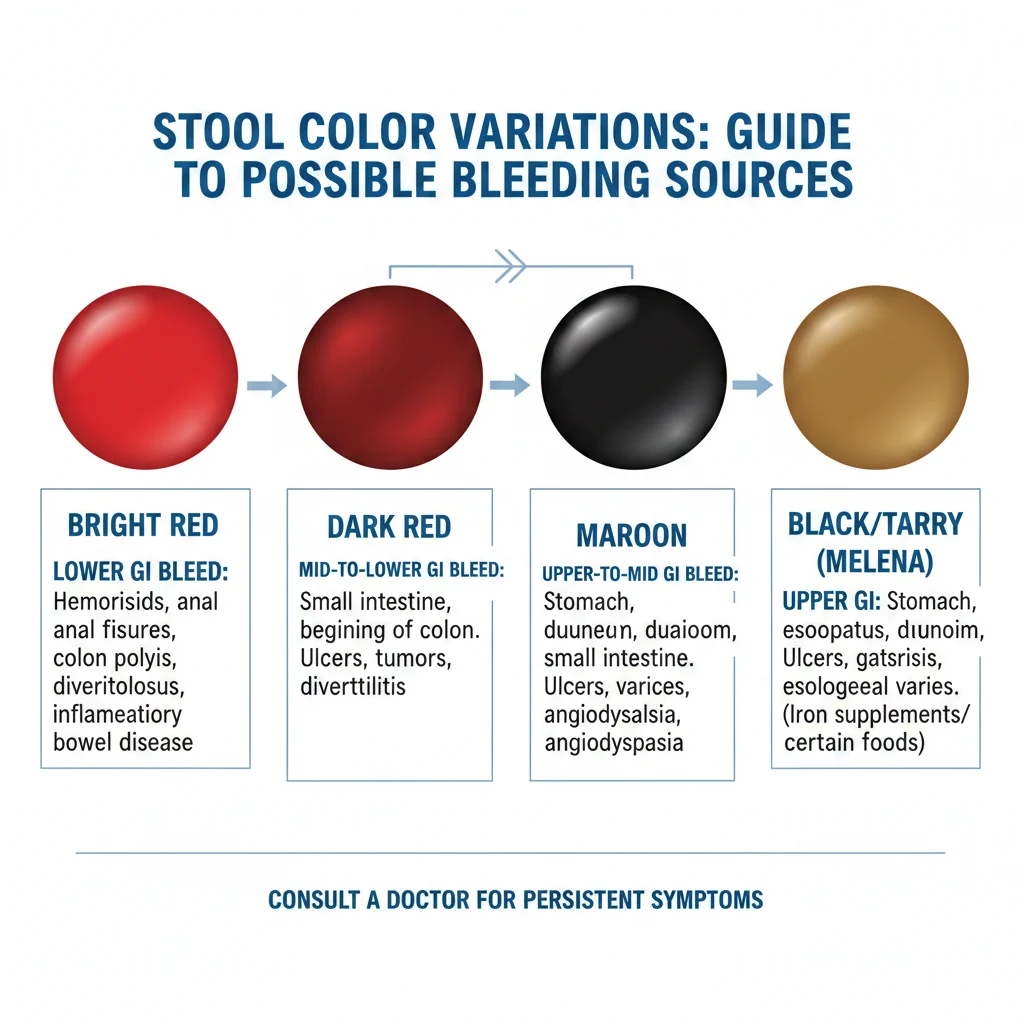
The color of blood in stool can provide important clues about the source of bleeding and the seriousness of the condition.
- Bright Red Blood – Typically indicates bleeding from the lower gastrointestinal tract, such as the rectum or anus. Common causes include hemorrhoids, anal fissures, or minor trauma. Bright red blood often appears as streaks or coating the stool, and may be noticed on toilet paper.
- Dark Red or Maroon Blood – This may suggest bleeding from the small intestine or upper colon. The slower transit time allows the blood to darken before being expelled. Conditions like diverticulosis or inflammatory bowel disease can cause this type of bleeding.
- Black or Tarry Stool (Melena) – Indicates digested blood from the stomach or upper GI tract, often caused by ulcers, gastritis, or stomach cancer. The stool may be sticky and have a strong, foul odor.
- Pink or Lightly Streaked Stool – Usually a sign of minor bleeding, such as from hemorrhoids, and is often less urgent, though persistent bleeding should still be evaluated by a doctor.
Understanding these color variations helps determine whether immediate medical attention is needed and guides the proper next steps for diagnosis.
Symptoms That May Accompany Blood in Stool
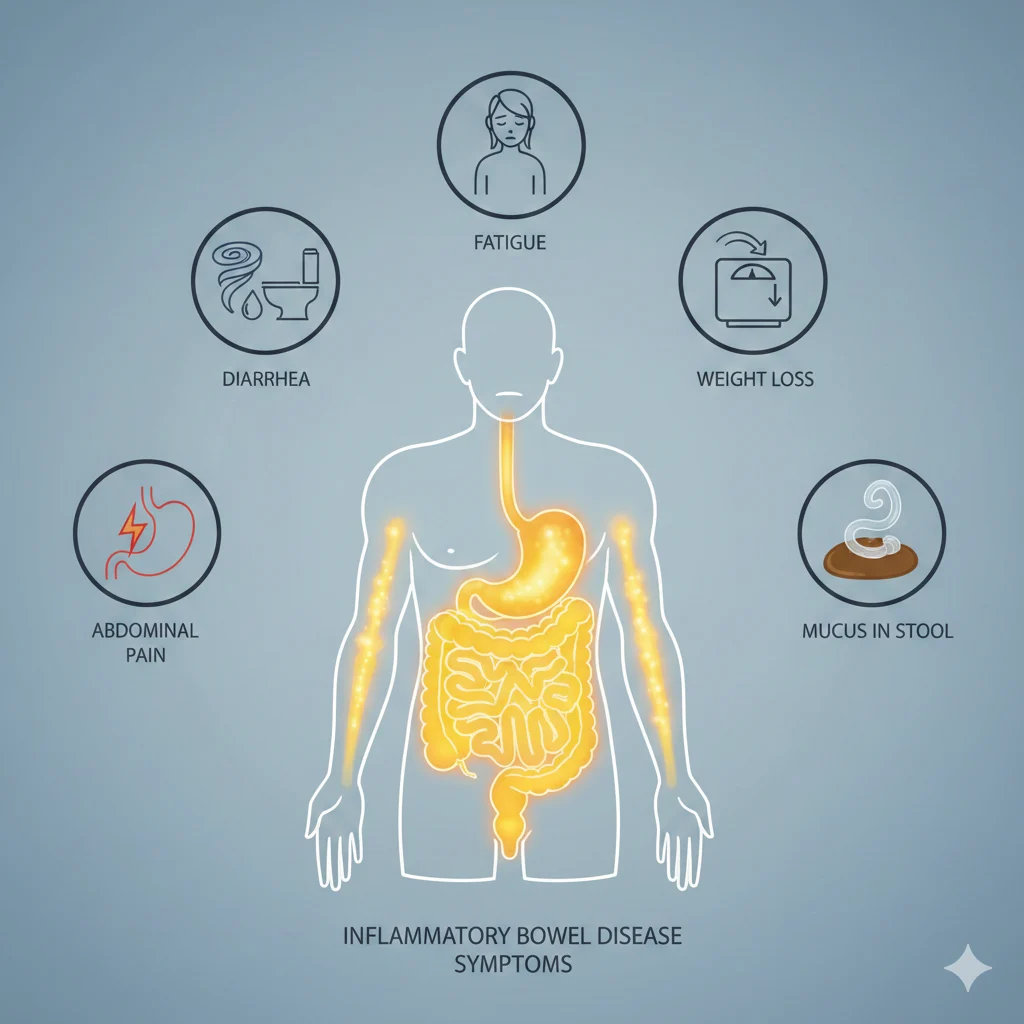
Blood in stool is often accompanied by other digestive or systemic symptoms, which can help indicate the underlying cause and urgency of medical care.
One of the most common accompanying symptoms is abdominal pain or cramping, which may be mild with hemorrhoids or severe with inflammatory bowel disease (IBD) or infections. Changes in bowel habits, such as diarrhea, constipation, or urgency, can also occur depending on the condition.
Fatigue or weakness may develop if bleeding is chronic, as blood loss can lead to anemia. Other signs of anemia include dizziness, pale skin, and shortness of breath.
Sometimes, blood in stool may be accompanied by mucus, particularly in cases of IBD or gastrointestinal infections. Unexplained weight loss, loss of appetite, or persistent bloating can signal more serious conditions, including colorectal cancer.
Recognizing these accompanying symptoms alongside blood in stool is crucial for early detection and timely medical evaluation, especially if the bleeding is persistent, heavy, or combined with any warning signs.
Risk Factors and Who Is Most at Risk

Certain people are more likely to experience blood in stool due to age, lifestyle, or underlying health conditions. Understanding these risk factors can help identify when to be extra vigilant.
Age is a major factor—people over 50 have a higher risk of colorectal cancer and other GI disorders that can cause bleeding. Family history also plays a role; individuals with relatives who had colon cancer, polyps, or inflammatory bowel disease are more susceptible.
Chronic constipation or frequent straining can lead to hemorrhoids or anal fissures, both common causes of bright red blood in stool. Similarly, a low-fiber diet can increase constipation, while poor hydration worsens stool hardness, increasing the risk of minor bleeding.
Other lifestyle factors include smoking, heavy alcohol consumption, and prolonged use of certain medications, such as NSAIDs or blood thinners, which can irritate the GI tract.
By recognizing these risk factors, individuals can take preventive measures and seek early medical attention when necessary, improving outcomes and overall digestive health.
Diagnosing Blood in Stool
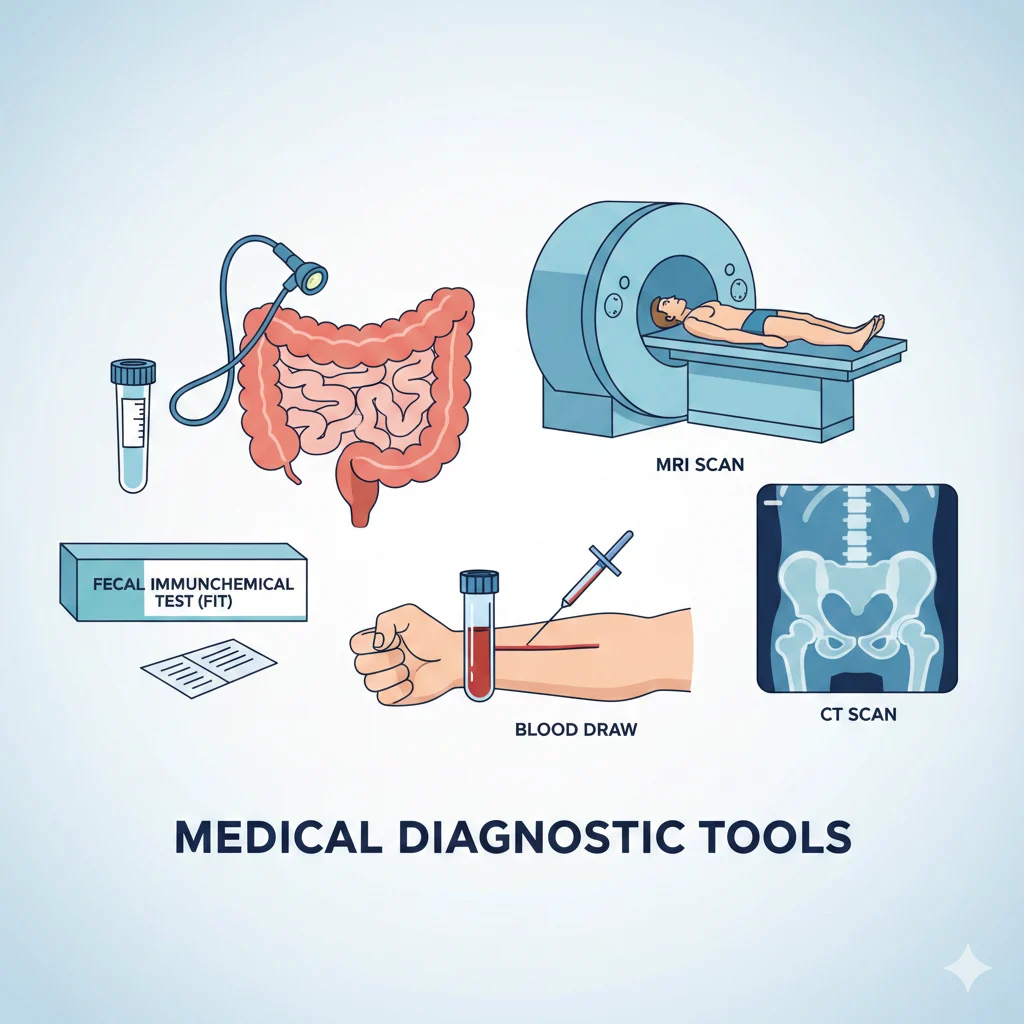
If you notice blood in your stool, a doctor’s evaluation is essential to determine the cause and appropriate treatment. Diagnosis often involves a combination of physical examination, lab tests, and imaging procedures.
Stool Tests
Doctors may begin with a fecal occult blood test (FOBT) or fecal immunochemical test (FIT) to detect hidden blood in stool that isn’t visible to the naked eye. These tests help identify bleeding in the gastrointestinal tract early, even before symptoms become severe.
Colonoscopy and Sigmoidoscopy
A colonoscopy allows doctors to examine the entire colon for polyps, tumors, or sources of bleeding, while a sigmoidoscopy focuses on the lower part of the colon. These procedures are crucial for diagnosing serious conditions like colorectal cancer and allow for biopsies or removal of abnormal growths.
Blood Tests
A complete blood count (CBC) can reveal anemia, which may result from chronic blood loss. Other blood tests check iron levels, inflammation markers, and overall health, providing clues about the underlying cause.
Imaging Tests
In some cases, CT scans, endoscopy, or capsule endoscopy may be recommended to visualize the upper gastrointestinal tract or small intestine, especially if bleeding is suspected from these areas.
Early and accurate diagnosis ensures timely treatment, reduces complications, and helps distinguish minor issues like hemorrhoids from serious conditions like cancer.
When to See a Doctor

Not all blood in stool is an emergency, but certain warning signs require prompt medical attention. You should contact a doctor immediately if you notice persistent or heavy bleeding, or if blood appears mixed with mucus or accompanied by diarrhea.
Severe abdominal pain or cramping, dizziness, fatigue, or shortness of breath, and unexplained weight loss are all red flags that may indicate a more serious underlying condition, such as inflammatory bowel disease or colorectal cancer. Even minor blood streaks that continue over time should be evaluated, especially if you are over 50 or have a family history of gastrointestinal disorders.
Additionally, if you experience black or tarry stools, this may signal upper GI bleeding and warrants immediate attention. Early consultation with a healthcare professional ensures proper diagnosis, treatment, and monitoring, potentially preventing complications and serious health risks.
Treatment Options Based on Cause
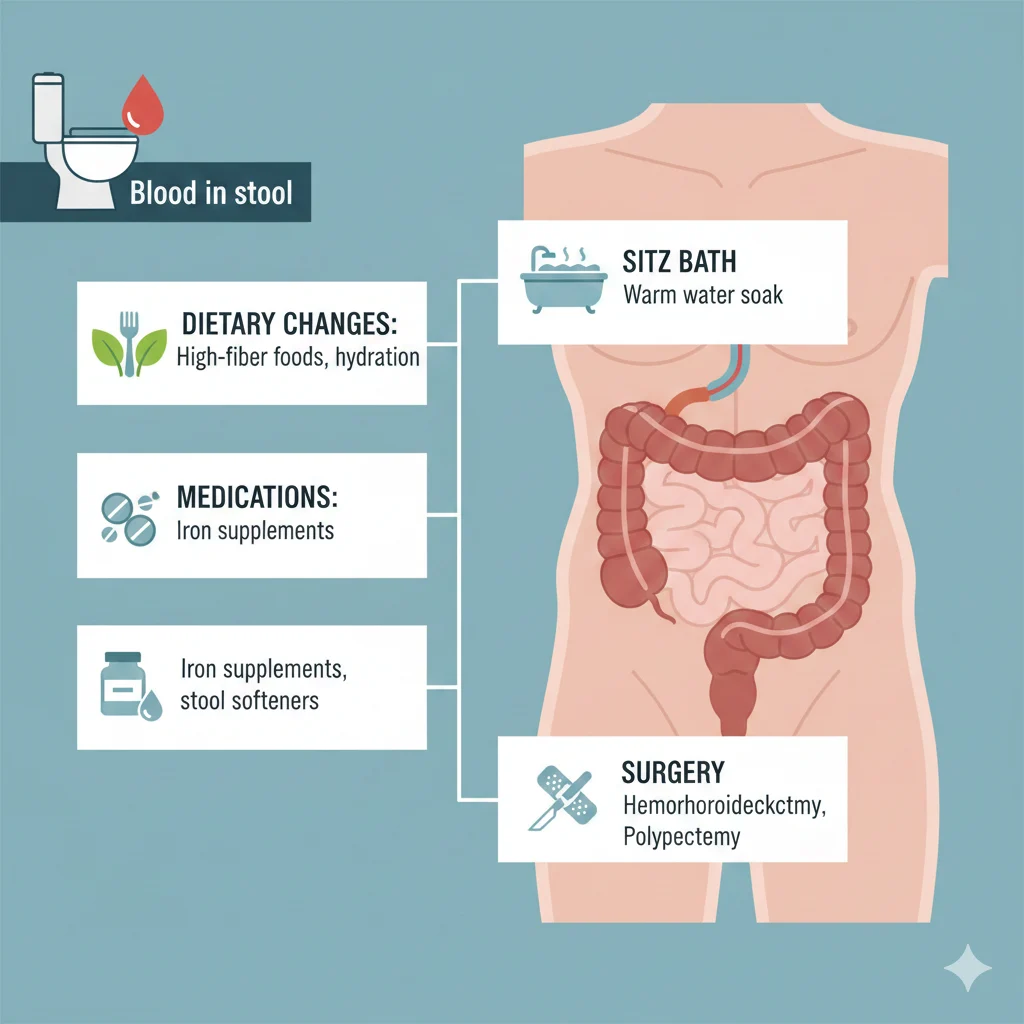
The treatment for blood in stool depends entirely on the underlying cause, ranging from simple lifestyle adjustments to medical interventions.
Hemorrhoids and Anal Fissures
Minor bleeding caused by hemorrhoids or fissures can often be treated with topical creams, sitz baths, and dietary changes. Increasing fiber intake and drinking plenty of water helps soften stools and reduce straining, preventing further irritation.
Gastrointestinal Infections
If an infection is causing bleeding, antibiotics or antiparasitic medications may be prescribed depending on the pathogen. Hydration and rest are essential to recover fully from diarrhea or GI upset.
Diverticulosis and Polyps
Bleeding from diverticulosis may require endoscopic procedures to control bleeding. Colon polyps are often removed during a colonoscopy to prevent progression to colorectal cancer.
Inflammatory Bowel Disease (IBD)
For conditions like Crohn’s disease or ulcerative colitis, treatment may involve anti-inflammatory medications, immunosuppressants, or biologics. Managing IBD reduces both bleeding and chronic inflammation.
Cancer-Related Bleeding
If colorectal or stomach cancer is detected, treatment may include surgery, chemotherapy, radiation, or a combination. Early diagnosis greatly improves outcomes.
Medication and Lifestyle Adjustments
If bleeding is caused by NSAIDs or blood thinners, your doctor may adjust dosages or recommend alternatives. Maintaining healthy bowel habits, avoiding prolonged straining, and staying hydrated are key preventive steps.
Proper treatment is guided by a medical professional and tailored to the cause, ensuring effective management and prevention of complications.
Prevention Tips for Blood in Stool

Preventing blood in stool often comes down to healthy digestive habits and regular monitoring. One of the most effective strategies is maintaining a high-fiber diet. Foods like fruits, vegetables, whole grains, and legumes help soften stool and reduce straining during bowel movements, which can prevent hemorrhoids and anal fissures.
Staying hydrated is equally important, as water keeps stool soft and promotes regular bowel movements. Avoiding prolonged sitting or straining on the toilet can also reduce pressure on rectal veins.
Regular exercise supports healthy digestion, improves circulation, and reduces constipation. For individuals over 50 or with a family history of GI disorders, routine screenings such as colonoscopies are critical for early detection of polyps, cancer, or other digestive conditions.
Additionally, moderating alcohol consumption, avoiding smoking, and using medications like NSAIDs responsibly can protect the gastrointestinal tract from irritation and bleeding.
By adopting these preventive measures, you can minimize the risk of blood in stool and promote overall digestive health.
FAQs About Blood in Stool
1. Is small blood streak in stool harmless?
Minor streaks of bright red blood are often caused by hemorrhoids or anal fissures and may not be serious. However, persistent bleeding should always be evaluated by a doctor.
2. How quickly should I see a doctor for bright red blood?
If you notice repeated bleeding, large amounts of blood, or accompanying pain, schedule a medical appointment promptly. Immediate attention is required for heavy or persistent bleeding.
3. Can stress cause blood in stool?
Stress alone typically doesn’t cause blood, but it can worsen digestive issues like constipation or IBS, which may indirectly lead to minor bleeding.
4. Does diet affect blood in stool?
Yes. A low-fiber diet can lead to constipation and straining, increasing the risk of hemorrhoids and fissures. A balanced diet with fiber helps maintain healthy bowel movements.
5. Is all blood in stool a sign of cancer?
No. While blood in stool can be a symptom of colorectal cancer, most cases are caused by minor conditions like hemorrhoids. Still, persistent or unexplained bleeding should always be evaluated.
6. Can medications cause blood in stool?
Yes. NSAIDs, aspirin, and blood thinners can irritate the GI tract and cause bleeding. Discuss alternatives with your doctor if this occurs.
Conclusion
Noticing blood in stool can be alarming, but understanding its appearance, causes, and associated symptoms can help you take timely action. Blood may appear bright red, dark red, maroon, or black, and its color often indicates the source of bleeding in the gastrointestinal tract.
While minor issues like hemorrhoids or anal fissures are common, persistent or unexplained bleeding could signal more serious conditions, including infections, inflammatory bowel disease, or colorectal cancer.
Recognizing accompanying symptoms such as abdominal pain, diarrhea, fatigue, or weight loss is crucial. Individuals with risk factors like age over 50, family history of GI disorders, or chronic constipation should be especially vigilant.
Medical evaluation, stool tests, colonoscopy, and imaging help accurately diagnose the cause, while treatment ranges from lifestyle changes and medications to surgery for serious conditions.
By adopting healthy digestive habits, a high-fiber diet, hydration, and regular screenings, you can reduce the risk of blood in stool and protect your digestive health. Early detection and preventive measures are key to maintaining long-term gastrointestinal well-being.